Clinical Intervention using Diabetes Project ECHO: A Case Based Outcome Study
Greta Jacobsen, MD, Phillip Kim, MD, MPH
SAMC Department of Family Medicine Residency Program
INTRODUCTION
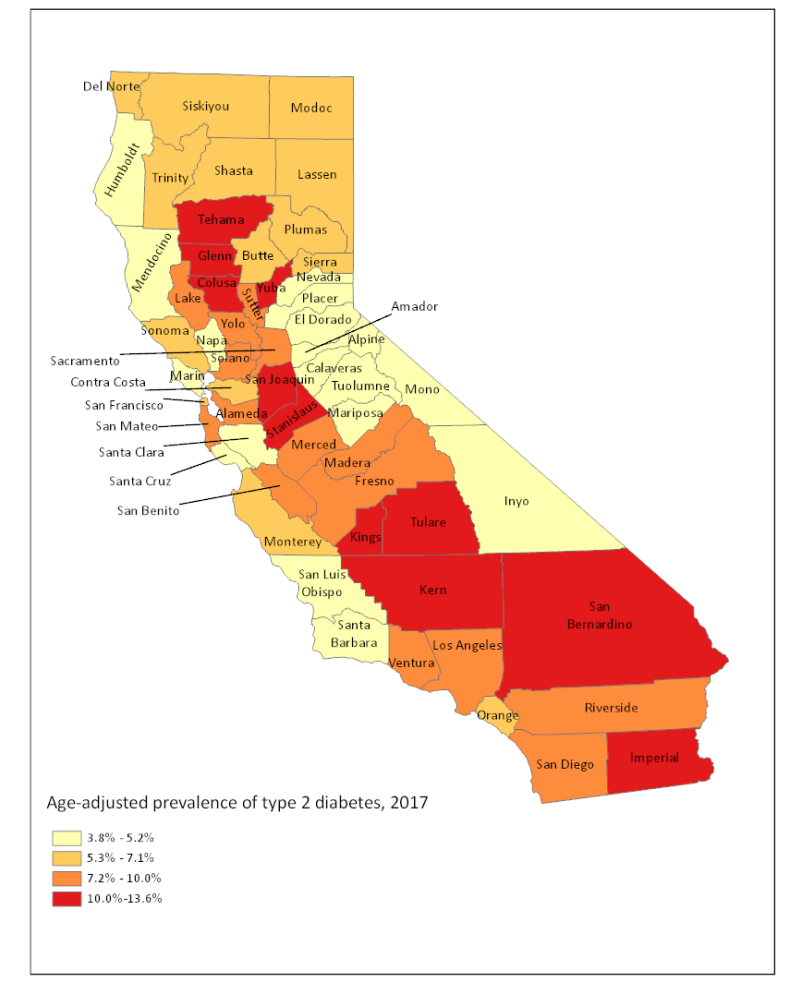
Type II diabetes mellitus is a chronic metabolic disorder which is characterized by persistent hyperglycemia. Type II diabetes mellitus is caused by resistance to insulin or impaired insulin secretion. Uncontrolled, it leads to long term sequelae in multiple organ systems with ensuing cardiovascular disease, nephropathy, neuropathy and retinopathy. In 2022, the CDC reported that 37.3 million persons had diabetes mellitus. More than 35 million of those persons had type II diabetes mellitus and 96 million, or 38 percent of the US population, had pre-diabetes. Between 2020-2021, 12.3 percent of the Fresno County population had a diagnosis of diabetes mellitus, above the national average of 11.3 percent.
The Saint Agnes Northwest Residency Clinic has had the opportunity to pair with Stanford’s ECHO Diabetes project. This program is a weekly tele-education and tele-mentoring collaborative. ECHO focuses on improving A1c control and decreasing hospital admissions/readmissions. The one hour tele-ECHO clinic sessions lend family medicine physicians the opportunity to learn and to present challenging insulin-requiring diabetes cases to a multidisciplinary endocrinology team at Stanford.
Family medicine physicians are the first line for management of diabetes mellitus. It is vitally important to take advantage of outside resources for additional help.
Prevalence of Type 2 Diabetes in California
CASE REPORT
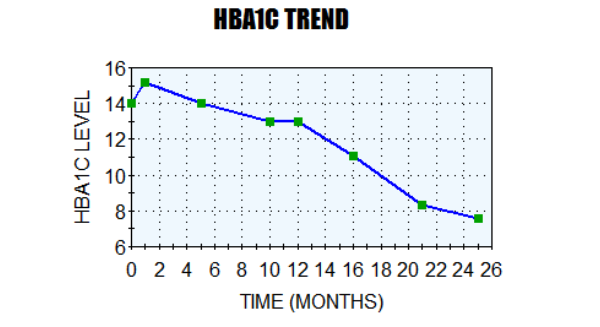
Patient's Clinical Journey and Outcome
Patient is a 58 year old female who initially presented to the Saint Agnes Northwest residency clinic in November 2020. Patient had previously been diagnosed with type II diabetes mellitus, but had not had access to medication after losing her insurance. Throughout a 2 year period of visits: November 2020 to November 2022, multiple issues were identified which presented challenges to achieving and maintaining control of diabetes: lack of access to insurance, poor understanding of disease, fear of medication and inability to present for follow up visits. Better control of diabetes mellitus was attempted through encouragement of regular, monthly follow up visits, in depth discussion with patient regarding disease and its long-term health effects and written information regarding carb counting and diabetes-friendly meals. This patient was presented to the Stanford ECHO team in January 2022.
- November 2020: POC glucose 357 and POC HbA1c 14.0% Patient commenced on Metformin 850mg BD, Basaglar 40u and Trulicity 0.75 once per week.
- December 2020: HbA1c 15.2.
- March 2021: POC glucose 593 and POC HbA1c 14.0 Patient not taking medication.
- August 2021: POC glucose 314 and POC HbA1c 13.0 Patient taking Metformin 850mg QD and Basaglar 40u for a few months. Patient not taking Trulicity.
- October 2021: POC HbA1c 13.0 Patient taking Metformin 850mg QD and Basaglar 40u. Patient not taking Trulicity. Metformin increased to 1000mg BID. Steglatro 5mg added.
- November 2021: POC glucose 365. Patient taking Metformin 1000mg BD, Steglatro 5mg QD, and Basaglar 40u. Patient not taking Trulicity. Ozempic 0.5mg once a week commenced. Steglatro increased to 15mg QD. Trulicity stopped due to poor record of use.
- December 2021: POC glucose 247 Patient taking Steglatro 15mg QD, Metformin 1000mg BID and Basaglar 40u. Patient not taking Ozempic.
- January 2022: → STANFORD PROJECT DIABETES ECHO INTERVENTION
- February 2022: POC Glucose 299. HbA1c 11.1% Patient taking Steglatro 15mg QD, Metformin 1000mg BID and Basaglar 40u. Patient not taking Ozempic.
- April 2022: Patient taking Steglatro 15mg QD, Metformin 1000mg BD and Basaglar 40u. Patient not taking Ozempic.
- May 2022: Patient taking Steglatro 15mg QD, Metformin 1000mg BID and Basaglar 40u. Patient taking Ozempic 0.5mg once per week. Ozempic increased to 1mg weekly.
- June 2022: Patient taking Steglatro 15mg QD, Metformin 1000mg BID and Basaglar 40u. Patient taking Ozempic 1 mg once weekly but not consistently.
- July 2022: POC glucose 132. HbA1c 8.3. Patient taking Steglatro 15mg QD, Metformin 1000mg BID, Basaglar 40u and Ozempic 1mg.
- August 2022: POC glucose 297 Patient taking Steglatro 15mg QD, Metformin 1000mg BID, Basaglar 40u and Ozempic 1mg once a week. Steglatro stopped. Jardiance 25mg QD commenced.
- September 2022: POC glucose 266 Patient taking Jardiance 25mg OD, Metformin 1000mg BID, Basaglar 40u. Not taking Ozempic.
- November 2022: POC glucose 217. Hb1A1c 7.6%. Patient taking Jardiance 25mg OD, Basaglar 40u, Metformin 1000mg BD and Ozempic 1mg every week. Ozempic increased to 2mg once per week.
CONCLUSION
Patients often struggle to control type II diabetes mellitus. In the case of this particular case, lack of understanding of the severity of disease, fear of injections, difficulty with changing diet and lack of access to Ozempic were some of the challenges preventing early diabetes control. One study showed that apprehension and fear of injections affect roughly 30% to 50% of patients with diabetes mellitus. This patient confided to our team that she was afraid of injecting herself, so had avoided certain prescribed medications. Studies have also shown the correlation between lack of understanding of diabetes and poor health outcomes. Unfortunately, low levels of health literacy are common in those suffering from diabetes mellitus, ranging from 15 to 40%. Each appointment entailed detailed discussions of long-term cardiovascular, renal and ophthalmological side effects of poor diabetes control. This was particularly important due to particular demographic risk in this case. Death from type II diabetes mellitus in Latinx populations is 1.25 times higher than non-Latinx populations. This challenge is amplified in Fresno County, where diabetes prevalence is high and specialist care is low. In the California Endowment report of 2006, it was reported that 75 percent of family care providers in Fresno had difficulty making referrals to endocrinologists for their Medi-Cal patients. Nationwide, it was reported that the shortage of adult endocrinologists will increase to ~2700 by 2025. This patient had Medi-Cal, with limited referral opportunities. Therefore, care was managed completely in the family medicine residency clinic. Lastly, the shortage in late 2022 and early 2023 of Ozempic, cause by a trend across the United States of usage of the medication for weight loss, reduced supplies for those with diabetes mellitus.
REFERENCES
- Diabetes Mellitus Type 2 - StatPearls - NCBI Bookshelf (nih.gov)
- Type 1 Diabetes Facts - JDRF
- National Diabetes Statistics Report | Diabetes | CDC
- Healthy Fresno County - Indicators - Adults with Diabetes (healthyfresnocountydata.org) J Epidemiol Glob Health. 2020 Mar; 10(1): 107–111.
- Recognition of and steps to mitigate anxiety and fear of pain in injectable diabetes treatment - PMC (nih.gov) Diabetes Metab Syndr Obes. 2015; 8: 49–56.
- Health literacy in diabetes care: explanation, evidence and equipment - PMC (nih.gov) Diabetes Manag (Lond). 2011 Mar; 1(2): 191–199.
- Exploring how patients understand and assess their diabetes control | (biomedcentral.com) BMC Endocrine Disorders volume 18, Article number: 79 (2018).
- Type 2 Diabetes Mellitus in Latinx Populations in the United States: A Culturally Relevant Literature Review - PMC (nih.gov) Cureus. 2022 Mar; 14(3): e23173.
- HPSA Cover.indd (fresnostate.edu)
- Trends in the Endocrinology Fellowship Recruitment: Reasons for Concern and Possible Interventions | The Journal of Clinical Endocrinology & Metabolism | Oxford Academic (oup.com) Volume 105, Issue 6, June 2020, Pages 1701–1706.

This is a well documented case study. Central California needs better diabetes care management. All family medicine doctors must be extensively trained in the pathology and treatment of this disease.
No comments to display
No comments to display