Evaluating the Role of Lipoprotein (a) and ASCVD 10-Year Risk Score in Coronary Artery Disease Outcome
Phillip Kim MD, MPH*, Chinedu Nwagwu MD, Ji Park MD, Anupama Poliyedath MD, Courtney Hill
SAMC Department of Family Medicine and Internal Medicine Residency Program
Fresno State University Graduate Statistics Studio
INTRO / BACKGROUND / PURPOSE
Introduction/Background
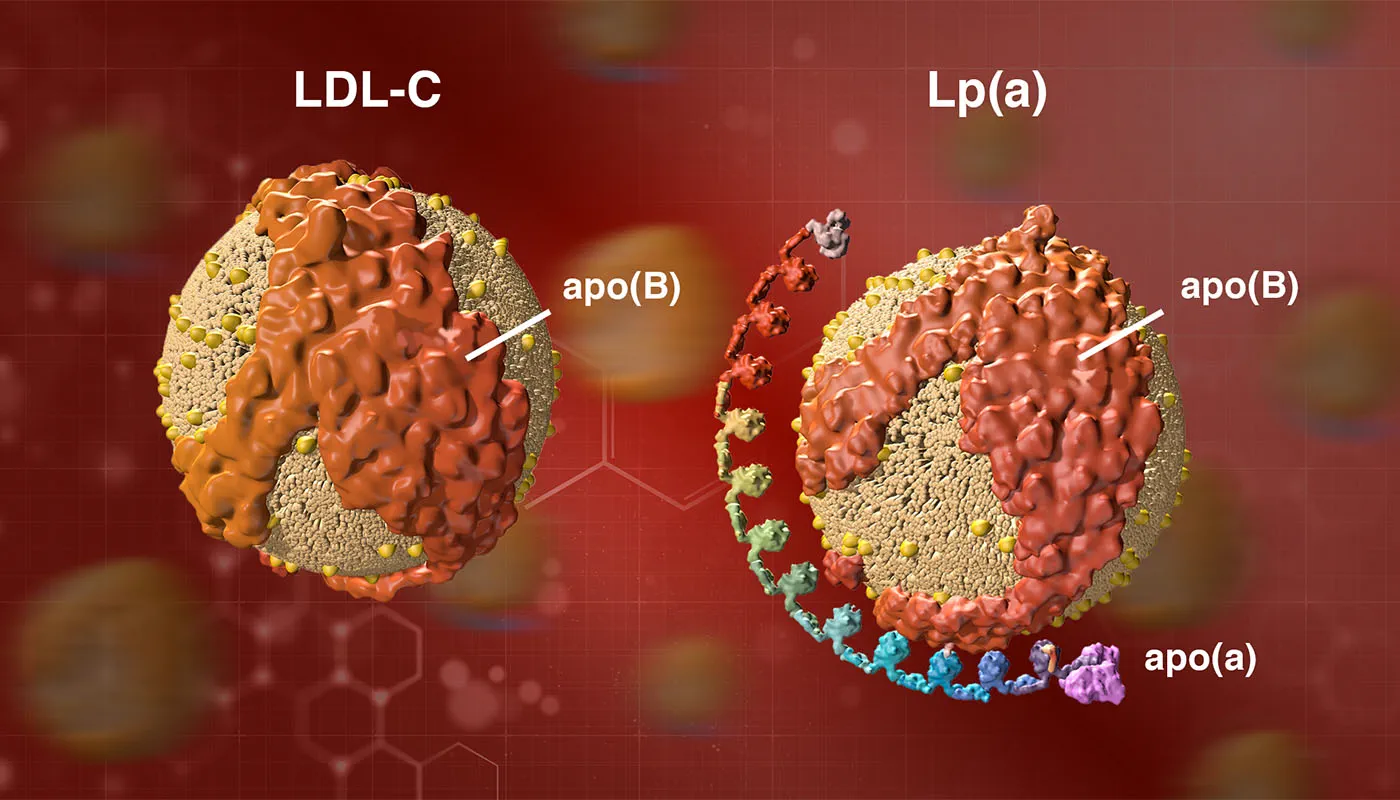
Lipoprotein A (Lp(a)) was discovered in 1963 as an apolipoprotein B (apoB)-containing lipoprotein. Lp(a)) is a low-density lipoprotein (LDL) cholesterol-like particle bound to apolipoprotein (a). This novel marker of cardiovascular disease acts through induction of vascular inflammation, atherogenesis, calcification, and thrombosis1. Evidence from mechanistic, observational, and genetic studies support a causal role of Lp(a) in the development of cardiovascular disease, including coronary heart disease and peripheral arterial disease, as well as aortic valve stenosis, and likely also ischemic stroke2. Lp(a) is a quantitative genetic trait with a very broad and skewed distribution, which is largely controlled by genetic variants at the LPA locus on chromosome 6q273. Lp(a) levels are estimated to be 90% hereditary. Elevated Lp(a) levels have been found to be predictive of ASCVD risk over 10 years4. One of the main obstacles to the clinical use of Lp(a) is that its measurement and target levels have not been standardized. Several available assays report results in mass (mg/dL) instead of concentration (nmol/L), the latter of which is preferred5. This is because lipoprotein “particle number” (molar concentration) has been found to be superior to component-based metrics for cardiovascular disease risk prediction6.
Purpose
The purpose of this retrospective cohort study is to investigate the relationship between (Lp(a), 10-year ASCVD risk score, and the incidence of coronary artery disease. By analyzing data from a large cohort of patients, this preliminary study aims to determine the predictiveness of Lp(a) levels and 10-year ASCVD risk scores for coronary artery disease and to assess their potential utility in identifying individuals at increased risk for this condition.
METHODS
Lp(a) Standardization
HEART UK Lp(a) Grade7 was utilized to identify patients with measured Lp(a) levels as follows:
- 32-90 nmol/L - minor
- 90-200 nmol/L - moderate
- 200-400 nmol/L - high
- > 400 nmol/L - very high
ASCVD 10-Year Risk Score
- <5% - Low risk
- 5-7.5% - Borderline risk
- 7.5-<20% - Intermediate risk
- >20% - High risk
Study Population
Outpatient SAMC Clinics:
- NW Physician Residency Clinic
- St. Agnes Care - Magnolia
- Avecinia -Clovis
- St. Agnes Care Brain and Spine
- St. Agnes Care IMA
Inclusion criteria:
- Using ASCVD 10-Year Risk Score guideline: Age (Years) 40-75
- Lp(a) nmol/L (2018-2023) via Quest/Labcorp
- Total Cholesterol (mg/dL), HDL (mg/dL)
- Race, Gender, Smoking Hx, Diabetes, HTN, HTN Treatment
- History of acute coronary event(s)
Statistical Methods
- Pearson Chi-Square (Bi Lp(a) Levels * ASCVD outcome)
- Binary Linear Regression Model (ASCVD Risk score * ASCVD outcome, Lp(a) *ASCVD outcome)
RESULTS
Patient Demographics
- Total Patients: 562
- Age Range: 40-75 (mean: 55.2, SD=9.9)
- Male: 49.1%
- Female: 50.9%
- White: 58.2%
- Black: 6.4%
- Other: 35.4% (Asian, Hispanic)
Risk Factors
- Non-Smokers: 66.2%
- Smokers: 33.8%
- HTN with treatment: 51.6%
- Diabetes: 26%
ASCVD outcome
Coronary Events: 12.8%
ASCVD Score and Risk Level
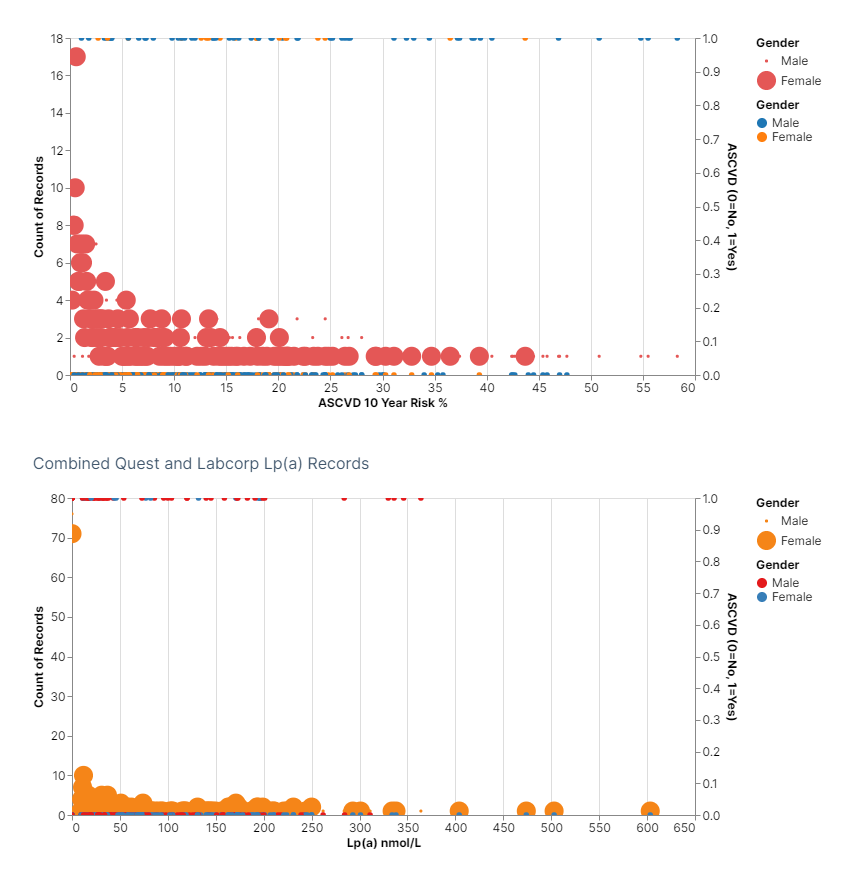
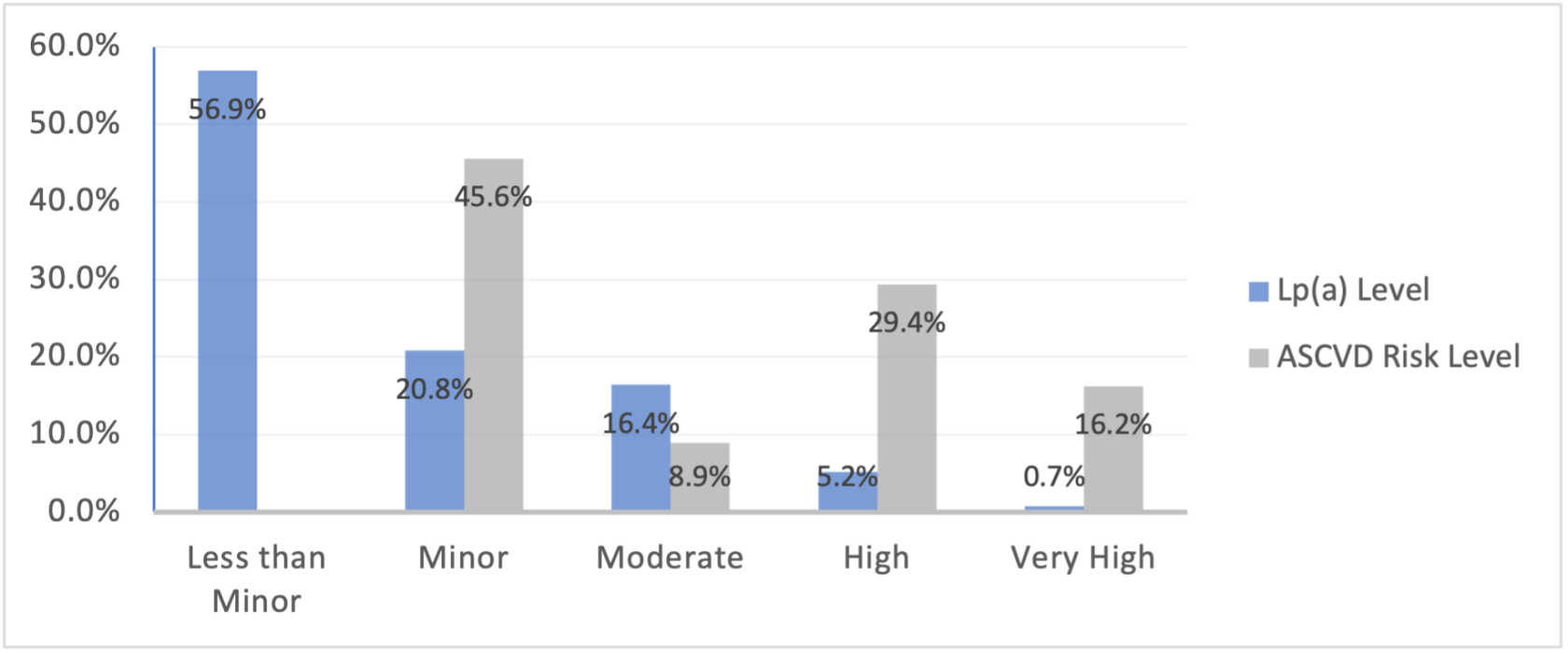
The mean ASCVD score for patients was 10.3 (SD=10.9) based on the ASCVD risk assessment. Based on the study categorization, the majority of patients fell into the low-risk category (45.6%), 8.9% were identified as having borderline risk, 29.4% as having an intermediate risk, and 16.2% were determined to be in the high-risk category.
Lp(a)
The mean of reported Lp(a) for patients was 55.2 nmol/L (SD=82.1 nmol/L). Based on the HEART UK grading system, 56.9% (320) of the sample was categorized as negligible, 20.8% (117) as minor, 16.4% (92) as moderate, 5.2% (29) as high, and 0.7% (4) were assigned to the very high category.
Pearson Chi-Square
Chi-Square tests of association were run to assess for a possible association between categorical variables ASCVD Risk Level and ASCVD event, as well as Lp(a) Level and ASCVD event. There is a statistically significant association between Lp(a) Level and ASCVD event, X(1) = 7.44, p < .01. A statistically significant association between ASCVD Risk Level and ASCVD event was also found, X(3) = 56.6, p < .001.
Binary Linear Regression
The logistic regression model was statistically significant, X2(4) = 60.06 with a p < .001. The model explained that patients with a high ASCVD risk score had an 18.9% increased risk of cardiac events in 10 years. Furthermore, this model correctly calculated risk at 87.2% of cases overall. This places ASCVD Risk score assessment as a significant predictor of having an ASCVD event with a p <.001. More extensively, those in the Intermediate Risk category being 4.7% more likely to have an ASCVD and those in the High-Risk category being 13.1% more likely to have an ASCVD.
Lp(a) Level is also significant, p <.01, with those having moderate, high, or very high Lp(a) levels being 2.2% more likely to have an ASCVD.
DISCUSSION / CONCLUSION
Despite converging evidence which identifies Lp(a) as an independent and causal risk factor for ASCVD, there are insufficient studies which compare Lp(a) to the ASCVD Risk Calculator to estimate a patient’s ASCVD risk.
In our study, we were able to re-demonstrate the association of the ASCVD Risk Calculator with ASCVD events (p<.001) consistent with prior studies and a statistically significant association between moderate, high, or very high Lp(a) level and ASCVD events (p<.01) with higher p-value compared to the ASCVD risk calculator.
Based on our findings, both elevated ASCVD risk score and elevated Lp(a) levels are independent risk enhancing factors for ASCVD concurring with multiple prior studies on literature. Our study also demonstrates the ASCVD score has stronger association with cardiovascular disease incidence compared to Lp(a), hence high ASCVD score is better predictor for ASCVD events.
These findings should be considered in the setting of limitations. Our sample size was limited which may decrease the statistical power. Second, the potential for confounding cannot be excluded such as race/ ethnicity differences. Third, given this is a cross- sectional study, temporal relationship cannot be determined. Ultimately, two major laboratory centers where our study collected data from utilize different methodology and reference ranges to measure Lp(a).
Further studies need to be conducted to interpret the elevation of both risk markers together and more aggressive ASCVD risk reduction strategies if there is an additive joint association.
REFERENCES
- Duarte Lau F, Giugliano RP. Lipoprotein(a) and its Significance in Cardiovascular Disease: A Review. JAMA Cardiol. 2022 Jul 1;7(7):760-769. doi: 10.1001/jamacardio.2022.0987. Erratum in: JAMA Cardiol. 2022 Jul 1;7(7):776. PMID: 35583875.
- Pia R Kamstrup, Lipoprotein(a) and Cardiovascular Disease, Clinical Chemistry, Volume 67, Issue 1, January 2021, Pages 154–166, https://doi.org/10.1093/clinchem/hvaa247.
- Kronenberg F, Utermann G. Lipoprotein(a): resurrected by genetics. J Intern Med. 2013 Jan;273(1):6-30. doi: 10.1111/j.1365-2796.2012.02592.x. Epub 2012 Nov 12. PMID: 22998429.
- Trinder M, Uddin MM, Finneran P, Aragam KG, Natarajan P. Clinical Utility of Lipoprotein(a) and LPA Genetic Risk Score in Risk Prediction of Incident Atherosclerotic Cardiovascular Disease. JAMA Cardiol. 2021;6(3):287–295. doi:10.1001/jamacardio.2020.5398.
- Wilson DP, Jacobson TA, Jones PH, et al. Use of Lipoprotein(a) in clinical practice: a biomarker whose time has come. A scientific statement from the National Lipid Association. J Clin Lipidol 2019;13:374-92.
- McConnell JP, Guadagno PA, Dayspring TD, Hoefner DM, Thiselton DL, Warnick GR, Harris WS. Lipoprotein(a) mass: a massively misunderstood metric. J Clin Lipidol. 2014 Nov-Dec;8(6):550-553. doi: 10.1016/j.jacl.2014.08.003. Epub 2014 Aug 19. PMID: 25499936.
- Cegla J, Neely RDG, France M, et al. HEART UK consensus statement on lipoprotein(a): a call to action [published online October 14, 2019]. Atherosclerosis. doi:10.1016/j.atherosclerosis.2019.10.011
- Ozen G, Sunbul M, Atagunduz P, Direskeneli H, Tigen K, Inanc N. The 2013 ACC/AHA 10-year atherosclerotic cardiovascular disease risk index is better than SCORE and QRisk II in rheumatoid arthritis: is it enough? Rheumatology (Oxford). 2016 Mar;55(3):513-22. doi: 10.1093/rheumatology/kev363. Epub 2015 Oct 15. PMID: 26472565.

No comments to display
No comments to display