Chronic Renal Failure
Definition
GFR <60 for 3 months or more
AND/OR
presence of kidney damage (albuminuria, sediment or anatomic abnormalities or a hx of kidney transplantation).
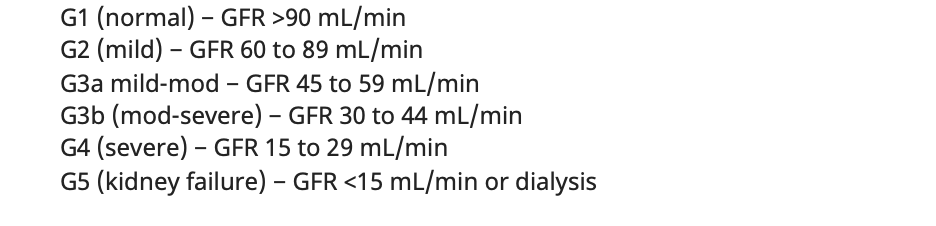
Stages of CKD:
Etiology:
Most common is DM. Others are HTN/RAS, glomerular, interstitial , drugs, congenital, myeloma and PKD.
Evaluation:
-Evaluate for uremic symptoms and signs
| General | Nausea, weight loss, hypothermia |
| Skin | Pruritus, calciphylaxis(skin ulcers) |
| Metabolic |
increased K and phosphorus, decreased Ca, 2 PTH, acidosis |
| Cardio | HTN, CHF, LVH, pericarditis |
| Neuro | seizures, neuropathy. decreased memory/attention/MS (encephalopathy) |
| Heme | Anemia, bleeding(plt dysfunction) |
Management:
-Consult Nephrology if proteinuria or GRF <30. BP measurements, IVs for dialysis access planning.
-Restrict sodium, potassium, phosphorus and protein intake especially if HTN or hyperkalemic.
-Treat/ risk reduction of co-morbidities (DM, HTN, CAD) with glucose control/ SGLTi, statin, ACEi/ARB ( reassess Cr and d/c if there is a 30% increase post ACEi/ARB).
-Sevelamer to control phosphorus levels, HCO3 replete if acidotic, Fe supplementation for anemia (goal Hb 10-11.5).
-Evaluate for transplant (GFR <20)

No comments to display
No comments to display